RESOURCES
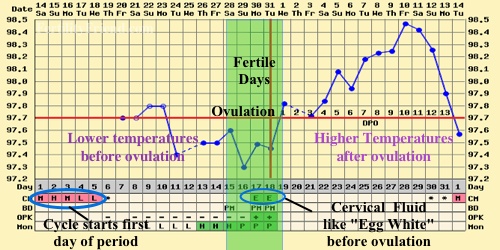
BBT Fertility Chart
Charting basal body temperature (BBT) is very important when a patient turns to acupuncture and Chinese medicine for fertility. The BBT chart is, basically, a chart on which your body temperature is being recorded each day in order to determine ovulation patterns. This chart is typically used to tell you whether you have ovulated or not and, if so, precisely which day you ovulated on.
The BBT chart is able to review a lot more information than you may think. A normal BBT chart for ovulation would show a biphasic pattern. During the follicular phase (prior to ovulation), temperature will usually be in the 97.0-97.5 range. After ovulation, the progesterone being released by the reproductive follicles cause temperature to increase by about 0.5-1 degree higher than the temperatureduring the follicular phase. The last day of low temperature is typically going to be the day that ovulation takes place.
The BBT chart is different from an ovulation prediction kit (OPK) because it is not meant to predict when ovulation will take place. The BBT chart is meant to be a confirmation of ovulation and to take the guesswork out of the process. Charting over the course of several cycles allows you to see a pattern in the cycles which helps tell you when the fertile days are in your particular menstrual cycle. Estrogen and progesterone levels can also be determined from your BBT chart.
Using the estrogen and progesterone levels, a health care professional is able to determine chi, blood, and fluid levels in addition to essence, in terms of Chinese medicine. The proper treatment is then based on the interpretation of those energetic elements. Whether the body is too warm or too cold, there is chi blockage, too much yin or yang (or the opposite), or anything else blocking ovulation can all be determined from the BBT chart. It is not simply a method of recording temperature. Proper herbs, acupuncture points, and moxibation treatment need to be applied at a specific point in your ovulation to balance things seen in your BBT chart. This is used for treatment guidelines.
To monitor your progress, the BBT chart can help indicate changes and improvements which may be taking place in your cycle so that the doctor can enhance or modify the treatment. This is a way to fine tune the treatment. It is a very useful tool for making an effective treatment plan for your specific condition.
In order to know how to chart BBT properly, go to www.fertilityfriend.com. There, you can get an online app and learn to chart your fertility. This is not meant to be stressful in any way. Try not to be too focused on the charting result. Just do it as a daily routine with a relaxed mind. Let your doctor to interpret it for you and create an effective treatment strategy.

Fertility Test
When should you seek help for fertility?
You should get a fertility workup if you:
- Are 35 or under and have been trying to conceive for 12 months
- Are 36 or older and have been trying to conceive for 6 months
- Don’t have regular menstrual cycles
- Aren’t sure if you are ovulating
- Have a history of Chlamydia (increases risk of blocked and/or damaged fallopian tubes)
- Suspect you have a problem
Fertility Testing For Women
History: A full physical and social history is essential. This includes doing a complete medical history, both past and present, such as developmental issues (eg. late onset of menstruation), use of medications, sexual history, use of proper lubricants, occupation (exposure to toxins), and emotional health.
Physical exam: This includes a BMI, blood pressure, secondary sexual sex characteristics exam, and pap smear.
The basic infertility workup consists of a series of tests that evaluate fertility factors, including:
- Ovulation
- Egg quality
- Fallopian tubes
- Health of the uterus
- Sperm
The following is a list of typical tests used to assess your fertility and prepare for pregnancy.
Ovarian reserve testing – There are several different ways to assess your ovarian reserve, such as:
- Day 3 FSH (follicle-stimulating hormone)
- Antral follicle count: If ovarian reserve or egg supply is in question, this simple ultrasound is often used
- Clomiphene citrate challenge
These tests are used to evaluate the health of your fallopian tubes and uterus
- Hysterosalpingogram (HSG)—This is a diagnostic X-ray that allows a study of your uterus and fallopian tubes.
- Hysteroscopy—this is a procedure where the doctor passes a hysteroscope—a narrow, telescope-like instrument with a camera on the end—through your vagina and cervix and into the uterus to directly examine the interior of your uterus.
Blood tests
- Prolactin High prolactin levels can suppress ovulation. It is generally associated with lactation but can be abnormally high for other reasons as well.
- Thyroid stimulating hormone (TSH) Thyroid evaluation varies greatly depending on the country, city and clinic; however, recent studies have shown that the ideal value for fertility are 2.5mIU/L.
- VZV IgG (to test chicken pox exposure)
- Rubella titre
- Complete blood count
- Blood type
- HIV, hepatitis B, hepatitis C, and syphilis testing
Additional blood tests
- APA: If you have a history of 3 miscarriages or more, it would be worthwhile to get tested for antiphospholip antibodies in your blood. These are more commonly found in women with a history of autoimmune disease.
- Day 21: This test is not done as often as the Day 3s and assesses levels of progesterone in your blood, basically let you and your healthcare provider know whether or not you have ovulated
- Ovarian Assessment Report: OAR’s are a more in-depth look at ovarian reserve. In addition to FSH and estradiol, the OAR measure inhibin B, Antimullarian hormones, and Luteinizing hormones. When reviewed together, a much more accurate assessment of the ovarian reserve and fertility potential can be achieved.
Tests to determine the health of your uterus and fallopian tubes
Hysterosalpingogram (HSG): This is an X-ray of your fallopian tubes and uterus, preceded by the injection of a dye which allows the visualization of both the uterus and fallopian tubes. Blockages or physical abnormalities in the tubes and uterus can be revealed through this procedure.
Hysteroscopy: This procedure is usually often done if there is suspicion of endometriosis, fibroids, or adhesions (Asherman’s syndrome).
Men's Fertility
Semen analysis includes
- Count
- Motility (movement)
- Morphology (shape)
Blood tests for infectious diseases
- HIV1 -antibody
- HTLV 1 antibody
- Hepatitis B-surface antigen
- Hepatitis C-antibody
- RPR
Sperm Evaluation
The semen analysis is the measurement of 4 different properties of a single ejaculate:
- “Volume” is the amount of the ejaculate measured in cc’s
- “Count” is the concentration of sperm, measured in million of sperm/cc
- “Motility” is the percentage of sperm that are moving, i.e. living
- “Morphology” is the percentage of sperm that are normal in shape
The “normal” values for these parameters are greater than 2cc in volume, 20 million/cc in concentration, 50% motility, and 50% morphology. The presence of white blood cells in the semen may indicate an infection of the prostate or urethra, even if no symptoms are present.
If the semen analysis is persistently abnormal, a urological exam, more specific sperm testing and hormonal testing are recommended. The urological examination will check for the presence of anatomical abnormalities (varicocele, congenital absence of the vas deferens). More specific sperm testing might include more stringent morphology testing (Kruger morphology), or testing for the presence of white blood cells or antibodies. Hormonal testing includes measurement of Prolactin, FSH and Testosterone.
Women's Fertility
Ovulation
At the beginning of the menstrual cycle, an egg begins to develop in the ovary. After approximately two weeks of growth, the egg is released or “ovulated.” Following ovulation, the ovary produces the hormone progesterone to prepare the lining of the uterus for implantation of the embryo.
How do you know if you are ovulating?
- The basal body temperature graph (BBT) detects ovulation by showing a rise in the temperature (usually to greater than 98 degrees). The temperature is taken orally for 3 minutes immediately upon awakening. Ovulation generally takes place within the 24 hours before the temperature elevation. The BBT is most useful for reviewing the timing of tests and intercourse/insemination but does not predict ovulation.
- Ovulation Predictor Kits (OPK) detect the LH hormone surge in the urine. LH is the hormone that triggers ovulation. These kits are the only method for predicting when ovulation will occur. For most kits, once a positive result is obtained, ovulation will occur within 24 hours. OPKs are most useful for confirming that an LH surge has occurred, and for timing of tests and intercourse/insemination.
- The serum progesterone test determines if the ovary is secreting sufficient hormone levels for optimal uterine preparation. The preferred progesterone level is 10 ng/ml or greater when measured 7-9 days after ovulation (as determined by BBT or urinary LH kit).
Hormonal Abnormalities
Abnormalities in the levels of other hormones can interfere with the normal process of growing and ovulating an egg. These hormones are routinely checked as part of the hormonal/ovulation evaluation and include TSH (thyroid) and Prolactin.
LH – Luteinizing Hormone
This is a test which is often done on day 3 of the cycle. Having a high LH level will result in increased ovarian testosterone production, altered estrogen production, and abnormalities with ovulation. If your LH is higher than the FSH by 2:1 ratio, it can indicate polycystic ovarian syndrome. Normal day 3 range: 7 mIU/mL
Estradiol
Measured on day 3 of the cycle. If elevated, estradiol can lower the FSH, thereby masking elevated FSH levels. This can happen in cases of low ovarian reserve or functional cysts. Estradiol can be low in conditions of low ovarian reserve. If you have estradiol over 294 pmol/L (or 80 pg/ml), you’ll have a lower chance of success with an IVF cycle since you will not respond to stimulation as well.
Progesterone
This is often measured on day 21. It is used to determine whether ovulation has occurred as a healthy corpus luteum produces progesterone. It is important to measure progesterone 7 days after your ovulation, measuring on day 21 only applies to women who ovulate on day 14. Levels higher than 16 nmol/L strongly suggest an ovulatory cycle.
Cortisol
Often measured in the morning, costisol can indicate the impact of stress on the reproductive system. Elevated cortisol can affect ovarian circulation and function. Normal levels: 250 – 850 nmol/L taken between 6-8 am. Low cortisol can be found in congenital adrenal hyperplasia. Normal levels for cortisol between 6-8:00 AM is 250-850 nmol/L, while later in the day it becomes 101-536 nmol/L.
Testosterone
The total level of testosterone in the system. If elevated, this can indicate polycystic ovarian syndrome. High testosterone can interfere with normal ovulation, often causing delayed ovulation or anovulation. But too low can negatively affect the ovarian function. Normal range for women is 0.3-4.0 nmol/L.
Free testosterone
The amount of testosterone that is not bound to carriers and is available to stimulate tissues. The higher this is. the more androgenic effect there is on the tissues. This can be elevated in PCOS and specific adrenal conditions such as non-classical congenital adrenal hyperplasia (non classical CAH). Normal range in women is 0.1-8.9 pmol/L.
Prolactin
A hormone normally elevated in nursing and pregnancy. If elevated in other situations, it can interfere with ovulation and fertility. It can be elevated due to stress, medications such as antidepressants or painkillers, thyroid disease, or pituitary conditions such as microadenomas. Normal range in women is 3.3– 26.7 ug/L.
Other Fertility Tests
DHT – Dihydrotestosterone
A form of testosterone which is very potent. DHT can be elevated in pcos or enzyme conversion disorders, resulting in androgen excess signs and symptoms. Serum testing for DHT is often unreliable.
Sex hormone binding globulin
Can be low in patients with androgen excess conditions such as pcos or hypothyroidism. Can be high in patients with non-classical CAH or hyperthyroidism. Normal range for the follicular phase is 24–200 nmol/L and for the luteal phase is 48–185 nmol/L.
HbA1C
A long termarker of insulin resistance and blood glucose control. Can be elevated in pcos. Marks the previous 3 months of blood glucose control. Normal range is 0.040–0.060.
DHEA – S
A precursor to hormones, most especially androgens. DHEA is made by the adrenal gland. Levels tend to reduce with age and can be reduced in low ovarian reserves. Levels can be elevated in PCOS. Normal range in women is 0-11 µmol/L.
Ferritin
A marker for stored iron. Levels can be low in patients with infertility. Ferritin levels of above 50 are recommended.
Egg Quality
FSH Follicle Stimulating Hormone
Day 3 FSH
What is a day 3 FSH?
One of the ways to evaluate your fertility potential is to measure the concentration of the follicle-stimulating hormone (FSH) on the 3rd day of your menstrual cycle. As a woman ages, the number of eggs in her ovaries declines. As the egg number or reserve declines, the FSH level increases.
What is a day 3 FSH test used for?
It helps predict how well you might respond to the fertility medications used in assisted reproductive technologies (ART) such as superovulation, IVF, and ICSI. The FSH level gives a rough idea of how your ovaries are responding and if you are approaching menopause.
Although day 3 FSH levels may vary from cycle to cycle, it is the highest level of FSH on day 3 that is associated with the potential outcome of treatment.
The methods used to measure the FSH level vary from clinic to clinic and thus the level above which the FSH is considered to be elevated vary among clinics. Most Vancouver IVF clinics like day 3 FSH levels to be below 10.
Your physician may use other estimates of ovarian or egg reserve such as a clomiphene challenge test or an antral follicle count.
Many women with high FSH become pregnant when egg quality and ovarian health is worked on, so having a high FSH is not untreatable.
FSH Levels (Day 3)
Excellent – less than 6 mIU/mL
Good – 9 mIU/mL
Low 10-13 mIU/mL
Very Low – above 13 mIU/mL
Antral Follicle Count
What is an antral follicle count?
An antral follicle count is a vaginal ultrasound examination of the ovaries used to determine the number of antral follicles in each ovary. An antral follicle is a tiny (2-10mm) fluid-filled structure that contains an immature egg. As a woman ages, the number of eggs or follicles in each ovary declines.
What is an antral follicle count used for?
Much like day 3 FSH testing, the antral follicle count (AFC) gives us an estimate of the number of eggs in your ovaries at a given time. An AFC is done prior to IVF or ICSI to help us predict how well you might respond to the fertility medications.
Your day 3 FSH level can vary from month to month while the AFC varies less so. There is no single number of antral follicles that is considered low or high – your age, medical history, and fertility history are all considered, along with your AFC, to estimate your ovarian reserve. Typically, an AFC of 10 is reassuring while an AFC of 5 is worrisome.
Clomiphene Citrate Challenge Test
What is a clomiphene citrate challenge test?
This test, called “a provocative test,” is used to assess the fertility potential or ovarian reserve function.
Who is a clomiphene citrate challenge for?
This test gives us more information about your ovarian reserve if you have:
- Borderline high day 3 FSH level
- History of poor response to the stimulation of egg growth in a previous cycle of an ART
- Increasing age
What does the test involve?
The test involves first measuring the cycle day 3 FSH and estradiol blood level. Then, after you take two tablets per day of clomiphene citrate (Clomid, Serophene) each morning from day 5 to day 9 of the cycle, we do a repeat measure of your FSH and estradiol blood levels on cycle day 10 (the day after completing the clomiphene tablets).
Special Ovarian Reserve Markers
AMH
Antimullerian hormones are produced by growing follicles and prevent premature recruitment of primordial follicles. The value of the amh generally correlates with the number of functional primordial and antral follicles remaining in the ovary. Generally, the higher the AMH, the more healthy follicles are in the ovary.
Antimullerian hormones can predict the age of onset of menopause with some degree of accuracy. Low AMH often does not give a good prognosis for IVF because IVF is based on the stimulation of multiple follicles – women with lower AMH tend to get fewer follicles during IVF stimulation. However, even if AMH is low, conception is possible, as even if there are not many follicles remaining in the ovary, their quality can be improved with treatments. Natural conception with low AMH can and does happen.
Normal Ranges of AMH Levels
Low 0.0 to 0.3 ng/ml
reduced 0.3 to 0.7 ng/ml
Satisfactory 0.7 to 3.5 ng/ml
High 3.5+ ng/ml
Inhibin b
A marker of ovarian function and reserve, this protein is secreted by small developing follicles and works to inhibit FSH levels, hence the name “inhibin.” This test is completed on day 3 of the cycle. As inhibin is secreted by the follicles, it can indicate the number of and function of the remaining follicles. This test is not widely available. A satisfactory level is above 65 pg/ml while a reduced level is below 65 pg/mL. However, Inhibin B is a spectrum and this line is a general guideline, not a strict cutoff. Like with AMH, even if inhibin B is low, conception is possible if the health of the remaining follicles is enhanced.
TSH -thyroid stimulating hormone
Though the normal range is 0.4 – 4 mIU/L, the ideal level is 1 – 2.5. If levels are above 3, and especially if thyroid antibodies such as antithyroglobulin and anti-thyroid peroxidase are present with signs and symptoms of hypothyroidism, there is a definite risk for fertility and a greater chance if miscarriage.
Other tests for ovarian health
Vitamin D
Important for overall health, hormone balance, and stress levels. Normal levels of 1, 25 hydroxy vitamin D are 40 -150 pmol/L
Homocysteine
A marker of inflammation and circulatory health. This test is only recently being found to be important for ovarian health. Elevated levels can be found in autoimmune conditions, ovarian aging and endometriosis. Normal range is 4.7 – 14.1 umol/L
INR
A measure of blood clotting. Blood which clots excessively may interfere with implantation. Can also be elevated in endometriosis or fibroids. Normal value for INR is 0.9 – 1.2
Anti-sperm antibodies
The presence of anti-sperm antibodies in women can destroy or damage the sperm before they have the chance to fertilize the egg. Around 5% of infertile women have these antibodies in their bloodstreams.
Anti-thyroid antibodies
These include antithyroid peroxidase and antithyroglobulin. If present, these antibodies will reduce fertility even if thyroid function is normal. They can cause alterations in thyroid function and also can be cross-reactive with ovarian tissue. If you have PCOS and don’t respond to clomid, you may have antithyroid antibodies.
Antinuclear antibodies
These antibodies are present in autoimmune diseases such as Lupus and Sjogrens syndrome.
Fallopian Tubes
Hysterosalpingogram
What is a hysterosalpingogram?
A hysterosalpingogram (HSG) is an X-ray test that looks at the inside of your uterus and fallopian tubes.
What is a hysterosalpingogram used for?
- A hysterosalpingogram shows:
- Abnormalities in the uterus or fallopian tubes
- Blockages preventing the egg from moving through a fallopian tube to the uterus
- Blockages preventing the sperm from moving into a fallopian tube and fertilizing the egg
- Problems on the inside of the uterus preventing a fertilized egg from attaching to the uterine wall
What does a hysterosalpingogram involve?
During a hysterosalpingogram, a radiologist injects a dye through a thin tube that is inserted through the vagina and into the cervix. The radiologist takes pictures using X-rays (fluoroscopy) as the dye flows through the uterus and into the fallopian tubes. If there is any blockage or problems with your uterus, this will show up on the X-ray.
Some women find this test to be quite “crampy,” so we suggest that you take 2 tablets of Ibuprofen (e.g. advil or Motrin) about one hour prior to the procedure.
Health Of The Uterus
Hysteroscopy
What is a hysteroscopy?
A hysteroscopy is a procedure where the doctor passes a hysteroscope—a narrow, telescope-like instrument with a camera on the end—through your vagina and cervix and into the uterus to directly examine the interior of your uterus.
What is a hysteroscopy used for?
This procedure is used to determine if you have any fibroid tumours, polyps, scar tissue, or other obstructions that could be affecting your fertility.
What happens during the procedure?
During the procedure, the doctor inserts the hysteroscope into your uterus and may inflate the uterus with gas or saline liquid to get a better view of the uterine interior.
If the doctor finds anything abnormal, he or she may remove a small sample for further examination. You don’t need to have an incision with a hysteroscopy, and most women recover within an hour or two.
Because many women find this test to be quite “crampy,” we suggest that you take 2 tablets of Ibuprofen (e.g Advil or Motrin) about one hour prior to the procedure.
Powered By Zenchange